| front |1 |2 |3 |4 |5 |6 |7 |8 |9 |10 |11 |12 |13 |14 |15 |16 |17 |18 |19 |20 |21 |22 |23 |review |
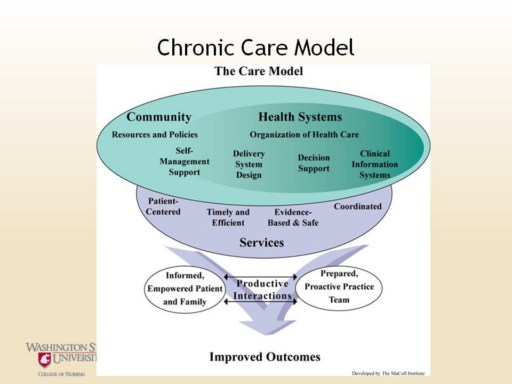 |
As shown in this depiction of the model, self-management support is a prominent component when care for chronic diseases is guided by the Chronic Care Model. Thus, there is overt recognition that people need support from their health care providers to engage in self-management activities.
All patients with chronic illnesses make decisions and engage in behaviors (self-management) that affect their health. Disease control and outcomes are largely dependent of the effectiveness of that self-management.
The goal of the Chronic Care Model is for patients and providers to work together to define problems, set priorities, establish goals, create treatment plans, and solve problems as they are encountered. To do so, patients must be ‘activated and informed’. To be activated and informed patients must have knowledge and behavioral skills. Thus, self-management, as purported by the Chronic Care Model, requires provider-patient partnerships and providers have the responsibility of ensuring patients are adequately supported to engage in self-management.
Included in these provider responsibilities are acknowledging that patients have a central role in their care, fostering among patients a sense of responsibility for their own health, and using evidence-based strategies to provide basic information, emotional support, and acquiring the skills needed to be positive self-managers. In so doing, patients and providers can have productive communication that will promote shared decision-making and better outcomes for patients with chronic conditions (e.g., Bodenheimer et al, 2002; Bray et al., 2005; Glasgow et al., 2002).
References: Chronic Care Model figure available at: http://www.improvingchroniccare.org/index.php?p=The_Chronic_Care_Model&s=2
Bodenhemimer, T., Lorik, K., Holman, H., Grumbac, K. (2002). Patient self-management of chronic disease in primary care. Journal of the American Medical Association, 288(19), 2469-2475.
Bray, P. , Roupe, M. , Young, S., Harrell, J., Cummings, D.M., & Whetstone, L.M. (2005). Feasibility and effectiveness of system redesign for diabetes care management in rural areas: The eastern North Carolina experience. Diabetes Educator, 31(5), 712-718.
Glasgow, R.E., Funnell, M.M., Bonomi, A.E., Davis, C., Beckham, V., & Wagner, E.H. (2002). Self-management aspects for the improving chronic illness care breakthrough series: Implementation with diabetes and heart failure teams. Annals of Behavioral Medicine, 24(2), 80-87. |